Supporting Second Victims
Over 250,000 hospital deaths result from medical errors in the US annually (Makary & Daniel, 2016). The Institute for Healthcare Improvement’s (IHI) landmark report, To Err is Human, defines medical harm as, "unintended physical injury resulting from, or contributed to by medical care (including the absence of indicated medical treatment), that requires additional monitoring, treatment, or hospitalization, or that results in death" (McCannon, Hackbarth & Griffin, 2007). These errors not only affect the patient and their loved ones but also impact the providers and are appropriately named the Second Victim Phenomenon.
Second Victim Phenomenon
In 2000, Wu coined the term second victim when describing the impact of medical errors on physicians, nurses, and interdisciplinary team members. Over the next decade the concept of second victims would evolve eventually clarifying that second victims include:
… healthcare providers who are involved in an unanticipated adverse patient event, in a medical error and/or a patient related injury and become victimized in the sense that the provider is traumatized by the event. Frequently, these individuals feel personally responsible for the patient outcome. Many feel as though they have failed the patient, second guessing their clinical skills and knowledge base (Scott, Hirschinger, Cox, et al., 2009).).
Second Victim Experiences
A recent systematic review by Chan et al. (2017) examining 30 international studies revealed similarities among the thoughts and feelings experienced by second victims following a medical error. Responses included feelings of guilt, distress, anxiety, fear, frustration, anger, and insufficiency. These psychological responses were reported as intense and long-standing. Scott et al. identified six stages that characterized the progression of the second victim phenomenon:

Supporting Second Victims
Understanding this psychological process, allows healthcare organizations to anticipate victim needs and provide necessary resources to support effective coping behaviors. Studies show that second victims need professionally trained counselors and formal support at the department/unit level (Chan, Khong and Wang, 2017; Scott et al., 2009). Providing emotional and informational support for the second victim is key.
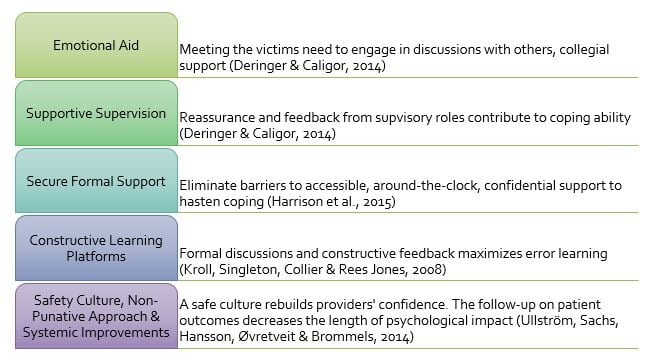
Organizational support structures are crucial in assisting second victims through the coping process. Many providers lack formal training regarding how to speak with patients and families when harm has occurred. According to Chan et al. (2017) support for second victims should include:
Government agencies have developed programs to assist organizations, for example:
- Agency for Healthcare Research and Quality (AHRQ) created an evidence-based toolkit designed to help providers discuss events in a “timely, thorough, and just way,” through the Communication and Optimal
Resolution (CANDOR) program. - Adverse Event Response Teams (AVERT) - Organizations adopting an AVERT model have demonstrated effectiveness in mitigating the harsh impact of medical errors on providers.
- IHI provides free recommendations for maintaining effective AVERT programs
- The Scott Three-Tiered Interventional Model of Second Victim Support (2010) is designed to create a successful Adverse Event Response Team:
- Tier 1: Promotes basic emotional first aid at the “local” or departmental level.
- Tier 2: Provides guidance and nurturing of previously identified second victims through use of specially trained peer supporters.
- Tier 3: Ensures prompt availability and access to professional counseling support and guidance when a second victim’s emotional stress exceeds the expertise of the peer rapid response team members.
While extensive efforts to reduce medical errors are underway, it is imperative that organizations educate staff on the second victim phenomenon and implement programs to support providers in times of need. To learn more about second victim support services, visit the resources listed below.
Resources:
Center for Patient Safety
Institute for Healthcare Improvement (IHI) - Adverse Event Response Team
Johns Hopkins RISE Program and RISE Case Study
Medically Induced Trauma Support Services (MITSS)
Second Victim Experience and Support Tool (SVEST)
References
Chan, S. T., Khong, P. C. B., & Wang, W. (2017). Psychological responses, coping and supporting needs of healthcare professionals as second victims. International nursing review, 64(2), 242-262. Deringer, E., & Caligor, E. (2014). Supervision and responses of psychiatry residents to adverse patient events. Academic Psychiatry, 38(6), 761-767. Donaldson, M. S., Corrigan, J. M., & Kohn, L. T. (Eds.). (2000). To err is human: building a safer health system (Vol. 6). National Academies Press. Harrison, R., Walton, M., Manias, E., Smith–Merry, J., Kelly, P., Iedema, R., & Robinson, L. (2015). The missing evidence: a systematic review of patients' experiences of adverse events in health care. International journal for quality in health care, 27(6), 424-442. Kroll, L., Singleton, A., Collier, J., & Rees Jones, I. (2008). Learning not to take it seriously: junior doctors’ accounts of error. Medical education, 42(10), 982-990. Makary, M. A., & Daniel, M. (2016). Medical error-the third leading cause of death in the US. BMJ: British Medical Journal (Online), 353. McCannon, C. J., Hackbarth, A. D., & Griffin, F. A. (2007). Miles to go: an introduction to the 5 Million Lives Campaign. Joint Commission Journal on Quality and Patient Safety, 33(8), 477-484. Rafter, N., Hickey, A., Condell, S., Conroy, R., O'connor, P., Vaughan, D., & Williams, D. (2014). Adverse events in healthcare: learning from mistakes. QJM: An International Journal of Medicine, 108(4), 273-277. Scott, S. D., Hirschinger, L. E., Cox, K. R., McCoig, M., Brandt, J., & Hall, L. W. (2009). The natural history of recovery for the healthcare provider “second victim” after adverse patient events. BMJ Quality & Safety, 18(5), 325-330. Scott, S. D., Hirschinger, L. E., Cox, K. R., McCoig, M., Hahn-Cover, K., Epperly, K. M., ... & Hall, L. W. (2010). Caring for our own: deploying a systemwide second victim rapid response team. Joint Commission journal on quality and patient safety, 36(5), 233-240. Ullström, S., Sachs, M. A., Hansson, J., Øvretveit, J., & Brommels, M. (2014). Suffering in silence: a qualitative study of second victims of adverse events. BMJ Qual Saf, 23(4), 325-331. Wu, A. W. (2000). Medical error: the second victim: the doctor who makes the mistake needs help too. BMJ: British Medical Journal, 320(7237), 726.




