Nightmare Bacteria: New CRE Superbug
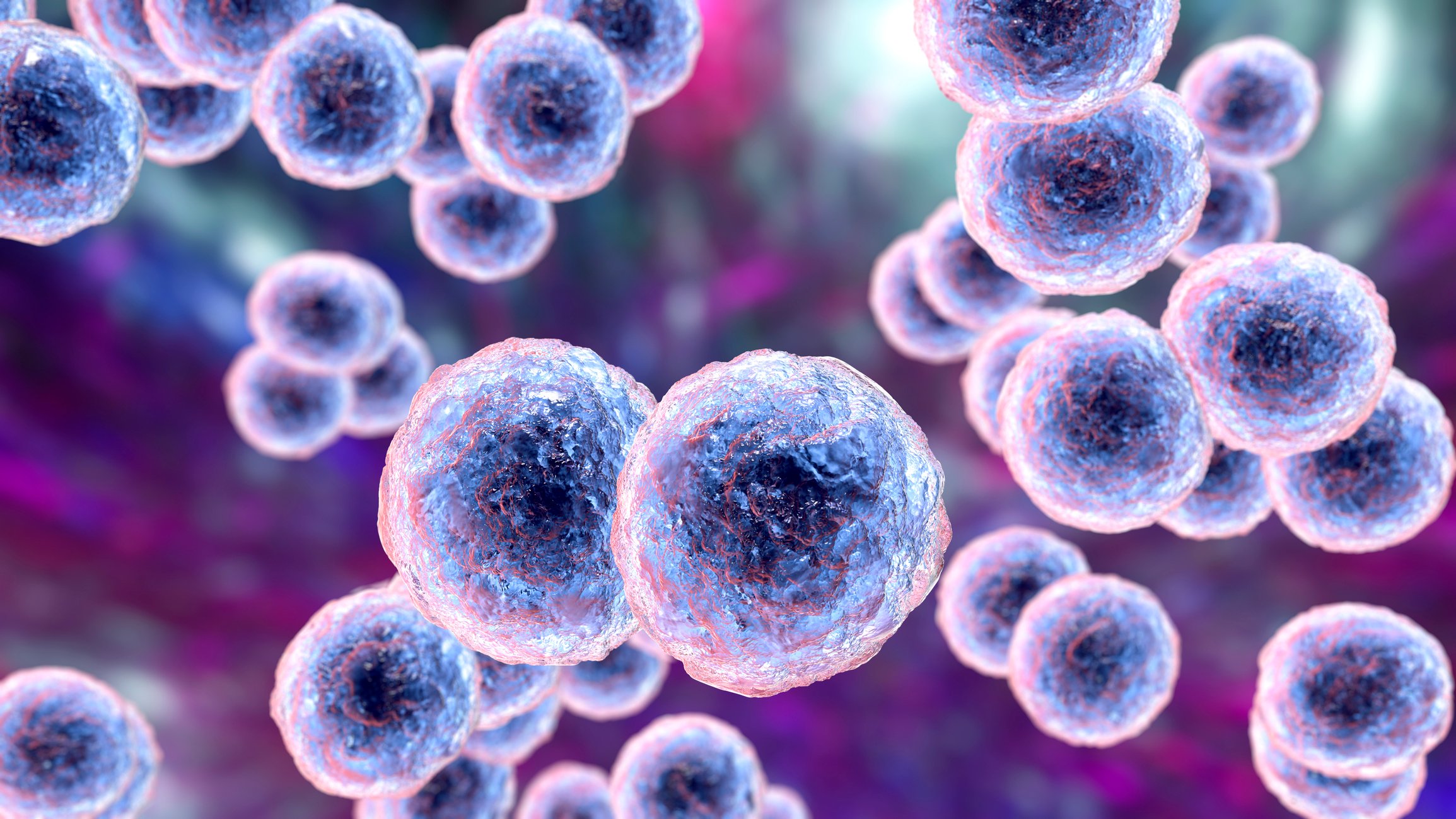
Carbapenem-resistant Enterobacteriaceae (CRE) are a group of relatively new multidrug-resistant organisms that are currently emerging in the U.S. Between 2001 and 2011, the percentage of CRE infections reported by acute-care hospitals in the United States increased almost fourfold (CDC, 2013a). These findings are significant because the bacteria can kill up to 50% of the patients who contract bloodstream infections from CREs (CDC, 2013b).
A Vital Signs report, released by the CDC in March 2013, issued a stern warning about CRE causing severe hospital-acquired infections (HAIs). According to this report, health care facilities in the Northeastern states have reported the most cases of CRE, with 42 states having had at least one patient test positive for the infection. In addition, one type of CRE, a resistant form of Klebsiella pneumoniae, has demonstrated a nearly sevenfold increase in prevalence, between 2001 and 2011, jumping from 1.6% to 10.4% (CDC, 2013b).
What is ‘nightmare bacteria’?
CRE has been dubbed the "nightmare bacteria" because it poses a triple threat. Not only are the bacteria resistant to all or nearly all antibiotics, but they also result in extremely high mortality rates. In addition, they have the ability to spread resistance to other bacteria, such as Escherichia coli, rendering E. coli resistant to antibiotic therapy as well (Brunk, 2013).
The good news is that healthcare professionals, especially nurses, have an opportunity to prevent the further spread of this superbug into the community (Brunk, 2013). The CDC is urging health care leaders, clinicians and health care departments to act aggressively to prevent the spread of CRE and alerting clinicians about the need to take additional preventative steps.
CRE Toolkit
The CDC has created a CRE Toolkit, which is posted online. In part, the CDC recommends that healthcare clinicians should:
- Ensure that patients with CRE infections be placed on Contact Precautions.
- Reinforce and evaluate adherence to basic hand hygiene practices.
- Screen epidemiologically-linked patient contacts for CRE colonization with stool, rectal or peri-rectal cultures. At a minimum, this should include persons with whom the CRE patient shared a room but could also include patients who were treated by the same healthcare personnel. A laboratory-based screening protocol is available here
- Ensure that a complete medical history accompanies the transfer of any patient infected with CRE. The CDC provides a sample transfer form, for general usage.
- Dedicate specific rooms and staff to CRE patients whenever possible; it is preferable that staff caring for CRE patients avoid caring for non-CRE patients.
- Remove temporary medical devices as soon as they are no longer needed.
- Prescribe and administer antibiotics judiciously as overuse and misuse increases drug-resistant infections.
- Pay particular attention to patients with a confirmed diagnosis of CRE infection, who have a history of an overnight stay in a healthcare facility outside the U.S. within the past 6 months. These patients should receive rectal screening cultures to detect CRE colonization and be placed on Contact Precautions while awaiting the results of these screening cultures.
References:
- Brunk, D. (2013). Nightmare CRE Infections on the Rise. Family Practice News. Retrieved from http://www.familypracticenews.com/news/infectious-diseases/single-article/nightmare-cre-infections-on-the-rise-cdc-says/a0206becb5b1bb3c1e20b4b81a11f78e.html
- Centers for Disease Control & Prevention [CDC]. (2013a).Healthcare-associated Infections (HAIs): Carbapenem-resistant Enterobacteriaceae (CRE). Retrieved from http://www.cdc.gov/hai/organisms/cre/
- Centers for Disease Control & Prevention [CDC]. (2013b). Vital Signs: Carbapenem-Resistant Enterobacteriaceae Morbidity and Mortality Weekly Report (MMW). Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w
© 2013. AMN Healthcare, Inc. All Rights Reserved.